
Are PTSD and Sleep Apnea connected?
Background: The empirical literature of network analysis studies of posttraumatic stress symptoms (PTSS) has grown rapidly over the last years.Objective: We aimed to assess the characteristics of these studies, and if possible, the most and least central symptoms and the strongest edges in the networks of PTSS.Method: The present systematic review, conducted in PsycInfo, Medline, and Web of.

Oorzaken van PTSS en de risicofactoren bondig weergegeven.
Psychogenic nonepileptic seizures (PNES) are nonepileptic events resembling seizures or syncopal attacks. The etiology, epidemiology, clinical features, and diagnosis of PNES are discussed in this review. Management and prognosis are reviewed separately. (See "Psychogenic nonepileptic seizures: Management and prognosis" .)

The Connection Between Sleep Apnea and PTSD Sleep Foundation
Participants' self-reported PTSS rates (57.1%) were high. PTSS and pain catastrophizing, but not exposure to PTEs, were related to chronic pain severity. Interestingly, a moderated mediation analysis indicated that the indirect effect of catastrophizing in the relation between exposure to PTEs and the number of somatic symptoms via PTSS existed.

Top 3 Tips to Service Connect Sleep Apnea Secondary to PTSD Is There Really a Connection? (The
Een functioneel-neurologisch-symptoomstoornis (FNS) is een motorische of sensorische verstoring, die niet verklaard kan worden vanuit een neurologische of andere somatische aandoening. Hierbij kan gedacht worden aan verlammingsverschijnselen, wegrakingen of abnormale schokkende bewegingen.
Sleep Apnea Secondary to PTSD VA Rating PTSD Lawyers
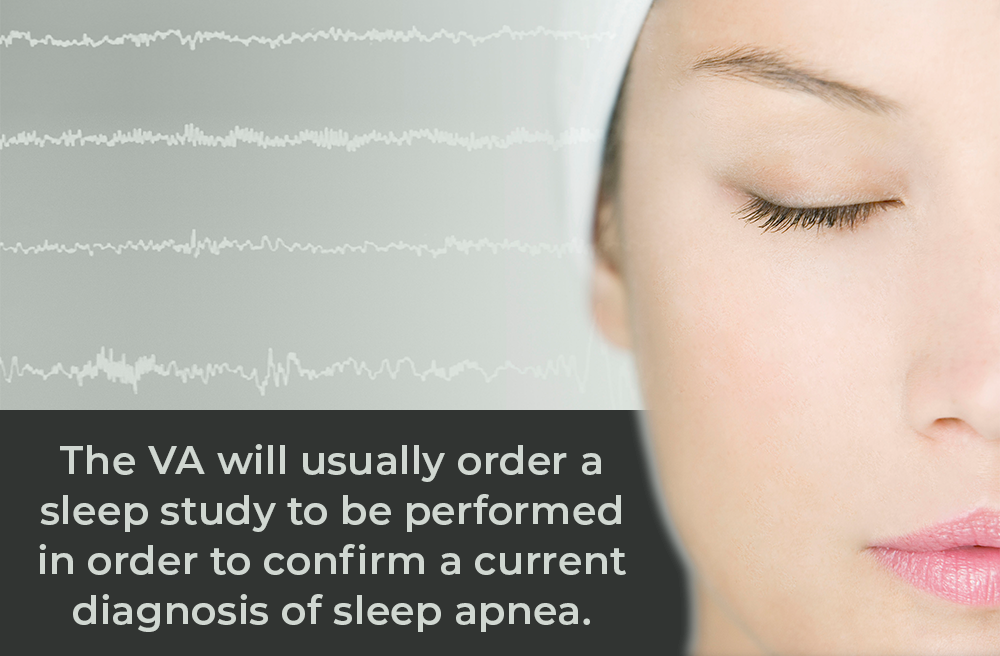
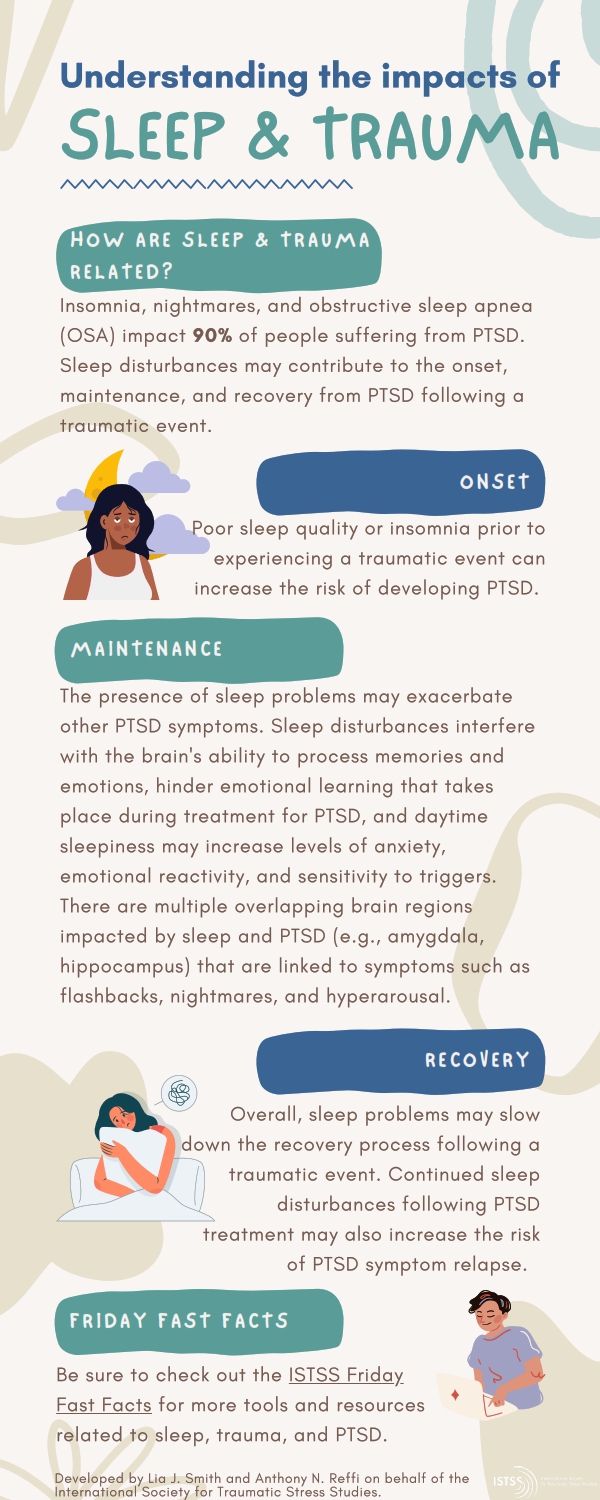
Sleep-disordered breathing can be a sign of untreated OSA, which is associated with worse symptoms of PTSD, as well as an increased risk of heart failure, dementia, and certain cancers. Sleep-disordered breathing is present in 95% of individuals who evacuated a fire, and 91% of victims who experienced consecutive crimes.
Sleep Apnea Secondary Connection to PTSD VA Disability Hill & Ponton, P.A.
Beyond the PTSD criterion symptoms of insomnia and nightmares, 40% to 98% of veterans with PTSD also have a co-occurring sleep disturbance such as obstructive sleep apnea (OSA), periodic leg movement disorder, sleep terrors, or nocturnal anxiety attacks. 4 - 6. OSA is one of the most common sleep disturbances, affecting between 5% and 10% of.
Sleep Apnea Secondary Connection to PTSD VA Disability Hill & Ponton, P.A.
Conclusions: In the absence of a clear precipitating brain injury, approximately one in six patients intubated for emergent convulsive symptoms had PNEA rather than SE. Although PNEA cannot be diagnosed only by the presence of these risk factors, these simple characteristics could raise clinical suspicion for PNEA in the appropriate setting.

Sleep apnea and PTSD linked to poor quality of life Study
16% of patients intubated for convulsive activity had psychogenic nonepileptic attacks (PNEA). • Six characteristics known on arrival can identify possible PNEA in this setting. • Patients with 5-6 of these risk factors had an 86% chance of having PNEA. • Care should be taken to avoid unnecessary intubation of these at-risk patients.
ISTSS Public Resources
Psychogenic non-epileptic attacks (PNEA) are behaviors described as a sudden, violent outburst or a fit of violent action or emotion. These attacks resemble epileptic seizures, but are caused by underlying psychological factors rather than by neurological or biomedical ones. What makes PNEA different from other non-epileptic conditions, which.

Understanding PTSD and Sleep Apnea
This can be helpful in allowing physicians to definitively identify whether someone has epilepsy or PNEA. Managing Stress . Whether you have PNEA or epilepsy, reducing the stress in your life can be helpful. According to the Epilepsy Foundation, 9 out of 10 people who actively manage their stress believe it has cut their risk of seizures.

sleepapneaandptsd Tabak Law, LLC
Een veelvoorkomend symptoom van conversiestoornis is PNEA (Psychogene Niet-Epileptische Aanvallen)* of spanningsaanvallen. Dit betekent dat je aanvallen hebt die erg lijken op epilepsie, maar ze gaan niet samen met epileptiforme activiteit in de hersenen.

Understanding PTSD and Sleep Apnea
Psychogenic non-epileptic attacks (PNEA) are behaviors described as a sudden, violent outburst or a fit of violent action or emotion. These attacks resemble epileptic seizures, but are caused by underlying psychological factors rather than by neurological or biomedical ones.
Top 3 Tips to Service Connect Sleep Apnea Secondary to PTSD Is There Really a Connection? (The
Posttraumatic stress disorder (PTSD) is a debilitating anxiety disorder reported in 25% to 30% of individuals experiencing a traumatic event.1Those with this syndrome. present with constellations of symptoms such as intrusive recollection, nightmares, hyperarousal, and disturbed sleep. According to the National Comorbidity Survey, the.
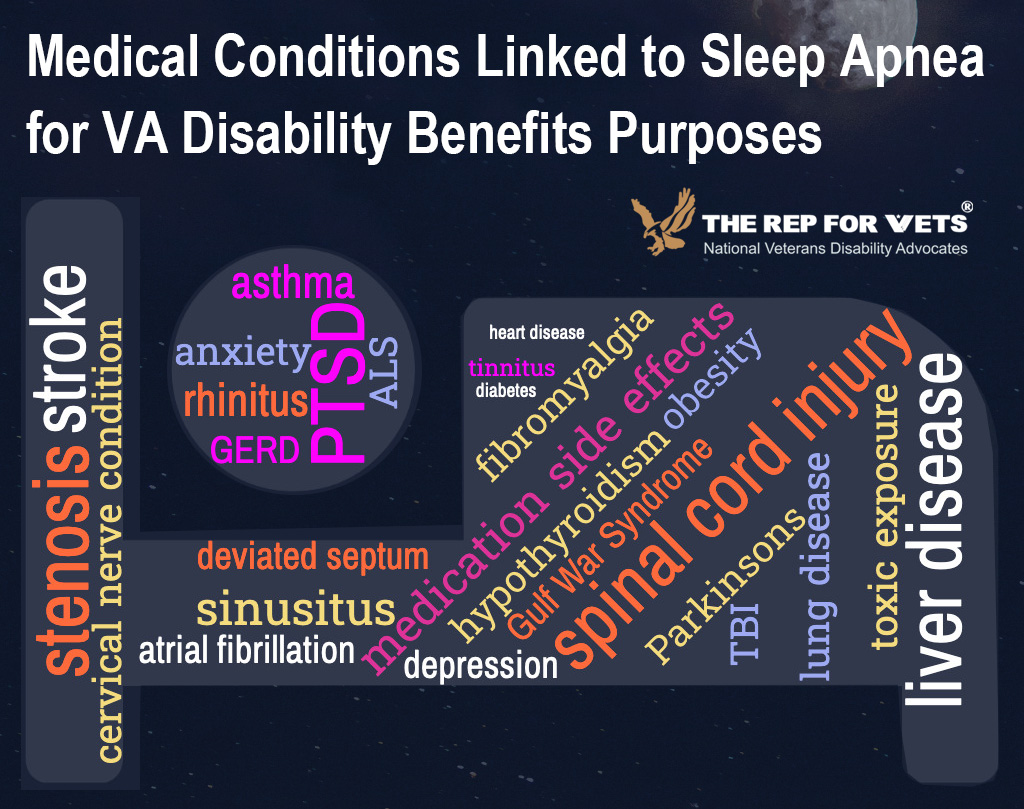
How to Claim Sleep Apnea Secondary to PTSD Rep for Vets
Om psychogene niet-epileptische aanvallen (PNEA) te behandelen wordt in het algemeen aanbevolen dat er een goede uitleg plaatsvindt waarom er geen sprake is van een somatische aandoening, zoals epilepsie. Ook moet worden besproken wat er wel aan de hand is (psycho-educatie) (Hall-Patch et al., 2010).

Clinical Importance of Sleep Disturbance as a Treatment Target in PTSD FOCUS
Psychogenic nonepileptic attacks (PNEA), also known as psychogenic nonepileptic seizures, dissociative seizures, or pseudoseizures (a term now widely considered pejorative), can be terrifying and frustrating for patients and their families. PNEA are transient episodes of involuntary movements or altered consciousness caused by psychological.

Top 3 Tips to Service Connect Sleep Apnea Secondary to PTSD Is There Really a Connection? (The
Rapid side-to-side head movements. Out-of-phase limb movements. Eyes-closed unresponsiveness. Pelvic thrusting. Changing patterns of movement. As PNES is associated with psychiatric conditions, people with PNES often have co-occurring psychiatric symptoms or diagnoses, such as a depressive mood or panic attacks.